Have you ever noticed tiny specks or cobweb-like shapes floating around in your field of vision? If so, you may have experienced Dry eyes and floaters. These mysterious little bugs seem to dart away whenever you try to focus on them, leaving many people wondering what they are and where they come from.
In addition to those pesky floaters, another common eye condition that affects millions of people worldwide is dry eyes. This uncomfortable condition can leave your eyes feeling irritated, gritty, and even cause blurry vision.
But what exactly causes these annoying issues? And is there any connection between them? In this blog post, we will dive into the world of floaters and dry eyes, exploring their causes, symptoms, treatment options, and how you can manage them effectively. So, let’s get started!
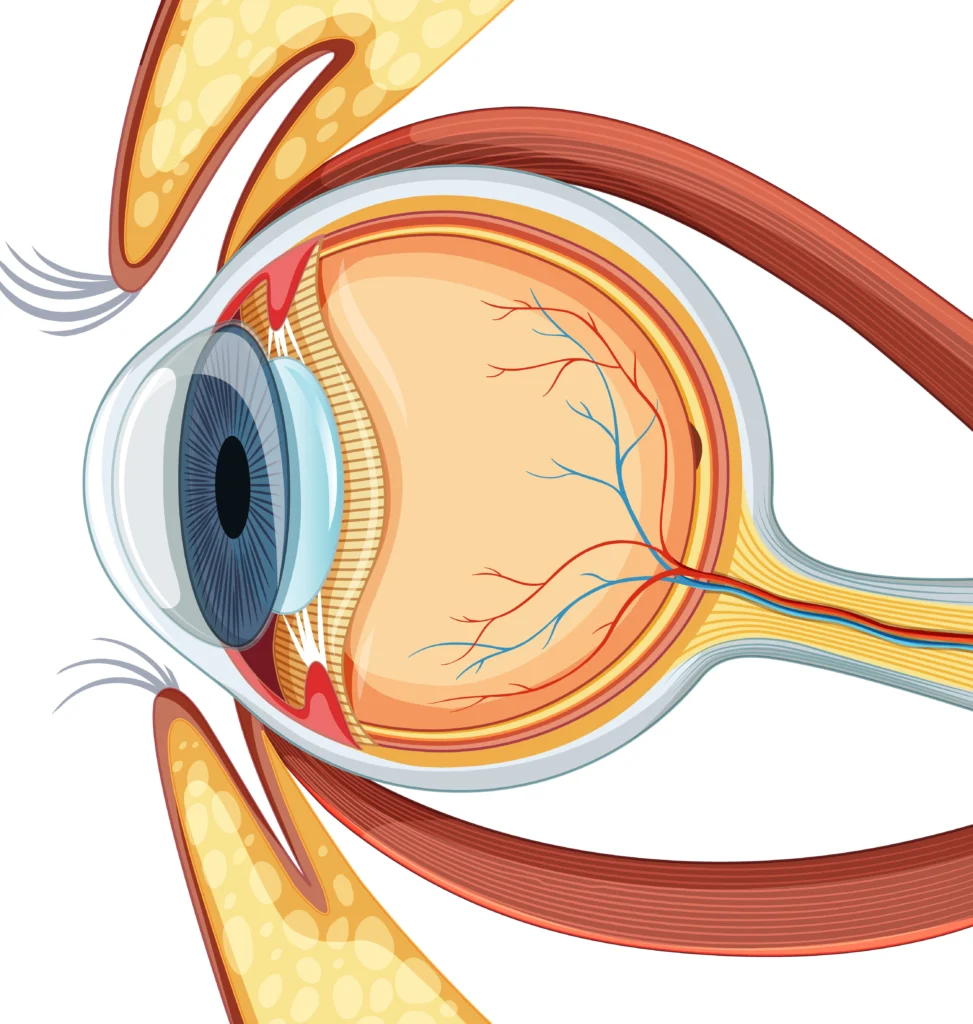
Table of Contents
Understanding Floaters
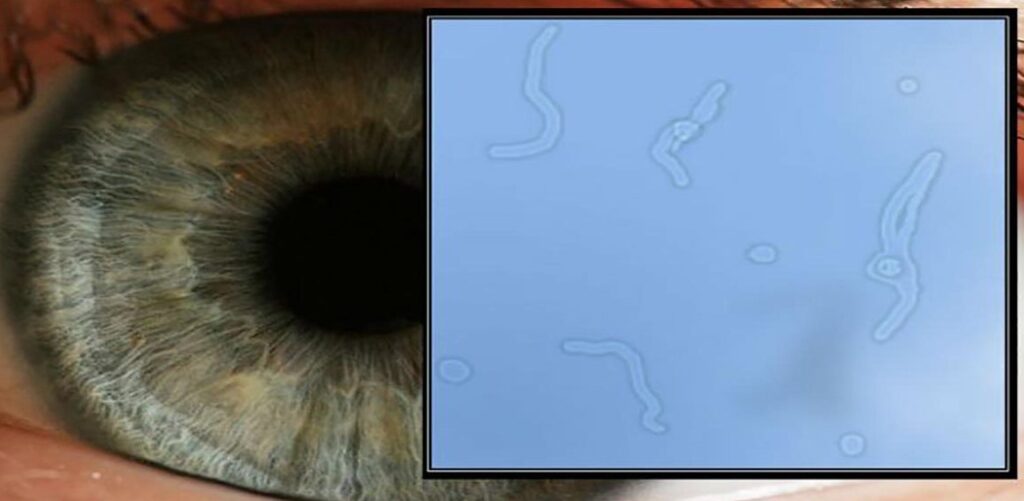
Floaters are tiny specks, spots, or cobweb-like shapes that appear to float in your field of vision. They may seem like bugs or particles drifting around, and they can be quite distracting. But what exactly are these floaters?
To understand floaters, we need to know a bit about the structure of our eyes. Inside the eyeball, there is a gel-like substance called the vitreous humor that helps maintain its shape. Over time, this gel can become more liquid and develop small clumps or strands.
When light enters our eyes and reaches the retina at the back of the eye, these clumps cast shadows on the retina which are then perceived as floaters in our vision. These shadows move along with eye movements and often appear more noticeable against bright backgrounds.
While most floaters are harmless and simply a natural part of aging, sometimes they can be caused by underlying eye conditions such as retinal detachment or bleeding within the eye. If you notice a sudden increase in floaters accompanied by flashes of light or changes in peripheral vision, it’s important to seek immediate medical attention.
In summary – understanding floaters requires knowing about the gel-like substance inside our eyes called vitreous humor that can form clumps and cast shadows on our retina causing those pesky little specks floating around in our vision!
Causes of Dry eyes and Floaters
Floaters are those tiny specks, strings, or cobweb-like structures that appear to float in our field of vision. They can be annoying and distracting, but what exactly causes them?
One common cause is the natural aging process. As we get older, the gel-like substance called vitreous inside our eyes becomes more liquid and starts to shrink. This leads to small clumps forming within the vitreous, casting shadows on the retina and causing floaters.
Eye injuries or trauma can also result in floaters. When there is bleeding in the eye due to injury or surgery, it may lead to the formation of floaters as blood cells become suspended within the vitreous humor.
Certain medical conditions can contribute to floaters as well. Diabetic retinopathy, where high blood sugar damages blood vessels in the retina; posterior uveitis, an inflammation of a layer at back of your eye; and retinal tears or detachment are some examples.
Nearsightedness (myopia) increases your risk for developing floaters because elongated eyeballs have a higher chance of experiencing changes in vitreous fluidity.
Understanding these various causes can help us better comprehend why we might experience those pesky floating specks!
Symptoms of Dry eyes and Floaters
Floaters are those tiny specks, strings, or cobweb-like shapes that seem to drift across our field of vision. While they may be common and usually harmless, they can occasionally be a cause for concern. Understanding the symptoms associated with floaters can help us differentiate normal occurrences from potential eye problems.
One of the most noticeable symptoms of floaters is seeing small dark specks or dots moving in front of our eyes. These floating spots often become more visible when looking at bright backgrounds such as white walls or blue skies.
Another symptom includes seeing string-like shapes drifting around. They may appear like cobwebs or thin strands that move along with our eye movements.
In some cases, individuals may also experience flashes of light alongside these floaters. These flashes could resemble lightning bolts or sudden bursts of brightness in their visual field.
It’s important to remember that while occasional floaters are generally not alarming, an increase in their frequency or sudden onset accompanied by other changes such as loss of peripheral vision should prompt a visit to an ophthalmologist for further evaluation and treatment options.
Stay tuned for the next section where we will explore possible treatment methods for dealing with floaters!
Treatment for Floaters
When it comes to treating floaters, the good news is that most cases do not require any specific treatment. In many instances, floaters will gradually fade or become less noticeable over time without any intervention. However, if floaters are affecting your vision and causing significant discomfort or interference with daily activities, there are a few treatment options available.
One potential treatment option is laser therapy. This involves using a focused laser beam to break up the floater into smaller pieces that are less visible or disrupt its movement in the eye. While this can be effective for some individuals, it’s important to note that laser therapy may not work for everyone and can carry certain risks.
Another option is vitrectomy surgery. During this procedure, the vitreous gel inside the eye is removed and replaced with a saline solution to eliminate floaters. Vitrectomy surgery is generally considered more invasive and carries higher risks compared to other treatments.
It’s crucial to consult with an ophthalmologist before considering any form of treatment for floaters as they can provide personalized recommendations based on your specific situation and medical history.
Exploring Dry Eyes and Floaters
Dry eyes are a common condition that occurs when your tear ducts don’t produce enough tears to keep your eyes lubricated. This can lead to discomfort and irritation, making it difficult to go about your daily activities.
The causes of dry eyes can vary, but some common factors include aging, hormonal changes, certain medications, environmental factors (such as dry air or wind), and underlying health conditions like diabetes or autoimmune disorders.
Symptoms of dry eyes may include a gritty or sandy feeling in the eyes, redness, itchiness, sensitivity to light, blurred vision, and even excessive tearing (as a result of the body’s attempt to compensate for the lack of moisture).
Fortunately, there are several treatment options available for managing dry eyes. These can range from over-the-counter artificial tears and eye drops that help lubricate the eyes to prescription medications or procedures like punctual plugs that help retain natural tears.
It’s important to consult with an eye care professional if you’re experiencing symptoms of dry eyes. They can provide a proper diagnosis and recommend appropriate treatment based on the severity of your condition.
Remember that prevention is key when it comes to managing dry eyes. Avoiding prolonged screen time without breaks, using humidifiers in dry environments, wearing protective eyewear outdoors on windy days – all these measures can help alleviate symptoms and promote better eye health.
Understanding and exploring the causes and symptoms of dry eyes is crucial in finding effective ways to manage this condition. By seeking professional advice and taking preventive measures such as incorporating lifestyle changes into our daily routines, we can minimize discomfort caused by dryness while keeping our precious vision clear and healthy
Causes of Dry Eyes
Dry eyes can be caused by a variety of factors, ranging from environmental conditions to underlying health issues. One common cause is reduced tear production. Tears are essential for maintaining the moisture and lubrication on the surface of our eyes. When there is a decrease in tear production, it can result in dryness and discomfort.
Certain medical conditions can contribute to dry eyes as well. Conditions like diabetes, rheumatoid arthritis, and thyroid disorders have been linked to decreased tear production. Other factors such as hormonal changes during menopause or pregnancy can also lead to dry eyes.
Environmental factors play a significant role in causing dry eyes too. Spending long hours staring at screens or working in air-conditioned environments can contribute to eye dryness. Additionally, exposure to smoke, wind, or dry climates may exacerbate the symptoms of dry eyes.
Some medications have side effects that include drying out the eyes as well. Antihistamines, decongestants, and certain blood pressure medications are known culprits.
It’s important to remember that everyone’s experience with dry eyes may differ based on their unique circumstances and lifestyle choices. By identifying the specific causes contributing to your condition, you will be better equipped to find appropriate treatment options moving forward.
Symptoms of Dry Eyes and Floaters
Dry eyes can cause a range of uncomfortable symptoms that can vary from person to person. If you’re experiencing any of the following, it may be a sign that you have dry eyes.
One common symptom is a persistent feeling of dryness or grittiness in the eyes. It may feel as if there’s something irritating your eye, like sand or dust. This sensation can worsen throughout the day, especially after long periods of reading or staring at screens.
Another symptom is redness and inflammation in the eyes. The blood vessels on the surface of the eye may become more prominent due to irritation and lack of moisture.
You might also experience excessive tearing as a result of dry eyes. Paradoxically, when your eyes are not producing enough tears to keep them lubricated, they may overcompensate by producing reflex tears which lead to watery eyes.
Blurry vision and sensitivity to light are other possible symptoms. When your tear film is unstable or lacking sufficient moisture, it can affect how well you see things clearly and make focusing difficult.
If you frequently wake up with crusty eyelids or notice an increased production of mucus around your eyes, these could be indications that you have dry eyes.
It’s important to note that these symptoms can also occur due to other underlying conditions, so it’s best to consult an eye care professional for an accurate diagnosis and appropriate treatment plan.
Treatment for Dry Eyes
Treating dry eyes involves a combination of self-care measures, lifestyle changes, and medical treatments. The goal is to relieve symptoms and improve the overall quality of tears.
Self-care measures include using artificial tears or lubricating eye drops to provide temporary relief from dryness and irritation. These drops can be used as frequently as needed throughout the day. It’s important to choose preservative-free eye drops if you need to use them more than four times a day.
In some cases, your doctor may recommend blocking the tear ducts to reduce tear drainage and keep the eyes moist for longer periods. This can be done with tiny silicone plugs that are inserted into the tear ducts or by cauterizing the tear ducts with heat.
Lifestyle changes such as avoiding environmental triggers like smoke, wind, and air-conditioning can also help manage dry eyes. Using a humidifier in your home or office can add moisture to the air and prevent excessive evaporation of tears.
For more severe cases of dry eyes, prescription medications like cyclosporine (Restasis) or lifitegrast (Xiidra) may be necessary. These medications work by reducing inflammation in the glands that produce tears.
It’s important to consult with an eye care professional who can determine which treatment options are best suited for your individual needs. Remember that managing dry eyes is an ongoing process, so it’s essential to follow up regularly with your doctor and make any necessary adjustments to your treatment plan.
Connection Between Floaters and Dry Eyes
Floaters are those tiny specks, cobwebs, or squiggly lines that seem to float across your field of vision. These visual disturbances can be quite bothersome and may interfere with daily activities. On the other hand, dry eyes occur when there is insufficient tear production or poor-quality tears.
Interestingly, there seems to be a correlation between floaters and dry eyes. Studies have suggested that people with dry eyes are more likely to experience floaters than those without this condition. This connection could be attributed to the fact that both conditions share similar underlying causes.
One possible cause is age-related changes in the vitreous humor inside our eyes. As we get older, this gel-like substance becomes more liquidy and can clump together, forming floaters. At the same time, aging also affects tear production and composition, leading to dry eyes.
Furthermore, certain systemic diseases like diabetes or autoimmune disorders can contribute to both conditions simultaneously. Inflammation plays a key role in these diseases and can affect various parts of the eye including the vitreous humor and tear glands.
It’s important to note that while there is a relationship between floaters and dry eyes, one condition does not necessarily cause the other. However, managing one condition effectively may help alleviate symptoms of the other.
Understanding the connection between floaters and dry eyes allows for better management strategies tailored specifically for each individual’s needs. Whether it involves addressing tear production or exploring treatment options for floaters such as laser therapy or surgery – finding relief from these visual disturbances is possible through proper diagnosis and care under professional guidance.
Managing Floaters and Dry Eyes
When it comes to managing floaters and dry eyes, there are several strategies you can employ to alleviate symptoms and improve your overall eye health. Here are some tips that may help:
1. Preventive Measures: To minimize the occurrence of floaters and dry eyes, it’s important to protect your eyes from harmful UV rays by wearing sunglasses with proper UV protection. Additionally, maintaining good hygiene by regularly washing your hands before touching your eyes can help prevent infections that may contribute to dryness.
2. Lifestyle Changes: Making certain lifestyle adjustments can also play a role in managing these conditions. Stay hydrated by drinking plenty of water throughout the day as dehydration can exacerbate dry eye symptoms. Incorporating omega-3 fatty acids into your diet through foods like fish or supplements may also be beneficial for both floaters and dry eyes.
3. Regular Eye Exams: Schedule regular visits with an eye care professional who can assess any changes in your vision or eye health over time. They will be able to provide guidance on how best to manage floaters and address any underlying causes of dry eyes.
Remember, while these techniques may offer relief for many individuals dealing with floaters and dry eyes, it’s always essential to consult with a medical professional for personalized advice based on your specific condition.
Preventive Measures
Taking proactive steps can help reduce the risk of developing floaters and dry eyes. Here are some preventive measures to consider:
1. Protect your eyes: Wear sunglasses or wide-brimmed hats when outdoors to shield your eyes from harmful UV rays and excessive glare.
2. Maintain a healthy lifestyle: Follow a well-balanced diet rich in omega-3 fatty acids, vitamins A, C, and E, as these nutrients are essential for good eye health. Stay hydrated by drinking plenty of water throughout the day.
3. Take regular breaks: If you spend extended periods on digital devices or performing close-up work, remember to take frequent breaks to rest your eyes and reduce strain.
4. Avoid smoking: Smoking has been linked to an increased risk of several eye conditions including dry eyes. Quitting smoking not only benefits your overall health but also helps protect your eyes.
5. Practice good hygiene: Wash your hands frequently and avoid touching or rubbing your eyes unnecessarily to prevent infections that could contribute to dryness or irritation.
6. Use artificial tears: If you experience occasional dryness or mild discomfort in the eyes, using over-the-counter artificial tear drops may provide temporary relief.
Remember that while these preventive measures can be beneficial in reducing the risk of floaters and dry eyes, it’s important to consult with an eye care professional for personalized advice based on your specific needs and conditions.
Lifestyle Changes
When it comes to managing floaters and dry eyes, making certain lifestyle changes can play a crucial role in improving your eye health. Here are some simple adjustments you can incorporate into your daily routine to alleviate the symptoms of dry eyes and reduce the occurrence of floaters.
Maintaining good overall hydration is essential for healthy eyes. Make sure you drink plenty of water throughout the day to stay properly hydrated. Additionally, incorporating foods rich in omega-3 fatty acids, such as fish, flaxseeds, and chia seeds into your diet can help promote optimal eye health.
Another lifestyle change that can benefit both floaters and dry eyes is reducing screen time. Spending long hours on digital devices not only strains your eyes but also contributes to dryness and irritation. Take regular breaks from screens and practice the 20-20-20 rule: every 20 minutes, look at something 20 feet away for 20 seconds.
Furthermore, protecting your eyes from harmful UV rays by wearing sunglasses when outdoors is crucial. Ultraviolet radiation can worsen both floaters and dry eye symptoms.
Quitting smoking is highly recommended if you have either condition. Smoking has been linked to an increased risk of developing various eye disorders including cataracts and macular degeneration.
Frequently Asked Questions about Floaters and Dry Eyes
1. Are floaters and dry eyes related?
Yes, there is a connection between floaters and dry eyes. When the eyes lack sufficient lubrication due to dryness, it can lead to an increased presence of floaters or make existing ones more noticeable.
2. Can eye strain cause both floaters and dry eyes?
Eye strain can contribute to the development of both floaters and dry eyes. Prolonged periods of staring at screens or reading without taking breaks can put a strain on your eyes, leading to these symptoms.
3. How do I know if I have floaters or just debris in my vision?
Floaters typically appear as small dots, squiggly lines, or cobweb-like shapes that move around when you try to focus on them. If you notice consistent objects floating across your field of vision, they are likely floaters rather than debris.
4. Can drinking more water help with dry eyes?
While staying hydrated is important for overall eye health, simply increasing water intake may not be enough to resolve chronic dry eye symptoms. It’s best to consult with an optometrist who can recommend appropriate treatments based on the underlying cause of your condition.
5. Are there any natural remedies for managing both floaters and dry eyes?
Some people find relief from mild cases of floaters by trying natural remedies such as gently massaging their temples or practicing eye exercises like focusing on distant objects regularly throughout the day.
For addressing mild cases of dry eyes, using warm compresses over closed eyelids and incorporating omega-3 fatty acids into your diet (found in foods like salmon and flaxseeds) may provide some relief.
However, it’s essential to remember that severe cases require professional medical intervention for effective treatment.
Conclusion
By making these simple lifestyle changes like staying hydrated, reducing screen time,
wearing sunglasses, and quitting smoking, you may be able.
to manage floater sand dry eyes more effectively and improve your overall ocular health.
Remember, talk to your eye care provider if the problems persist or worsen.
Mesothelioma Treatment Options, please do visit our website.